What’s the difference between anxiety and OCD?
The human mind is a powerful machine, but sometimes its gears get stuck, leading to cycles of excessive worry and distress. Obsessive-Compulsive Disorder (OCD) and Generalized Anxiety Disorder (GAD) are two distinct conditions that involve significant anxiety, yet manifest in profoundly different ways. Understanding these differences, recognizing the symptoms in everyday life, and knowing when and how to seek professional help are crucial steps toward regaining control and improving quality of life.
Anxiety Disorder vs OCD
Understanding Generalized Anxiety Disorder (GAD)
Both OCD and GAD share the common thread of anxiety, but their core mechanisms are unique. GAD is defined by excessive, uncontrollable worry about typical, everyday matters.
- Excessive Worry: The worry is constant, intense, and often shifts focus—from finances and health to work, relationships, or safety. People with GAD struggle to control their “what if” thought spirals, even when there is no immediate threat.
- Physical Symptoms: GAD is accompanied by chronic physical symptoms of tension, such as fatigue, irritability, sleep disturbances, muscle tension, and difficulty concentrating.
Unlike OCD, GAD does not involve compulsions or rituals. The anxiety is the disorder itself, a pervasive state of worrying about real-life concerns, rather than a reaction to an intrusive, specific obsession.
What Anxiety Looks Like and How it Creates Problems
While OCD focuses on a distinct obsession-compulsion loop, generalized anxiety is a state of chronic alarm.
The Pervasive “What If” Spiral
An individual with GAD constantly worries about their finances, even when their budget is stable. They spend hours every week running mental scenarios: “What if I lose my job? What if the stock market crashes? What if I run out of savings?” The worry is like a spotlight that jumps from one topic to the next without rest.
- Problem Created: This non-stop mental churning leads to exhaustion. The constant state of alert prevents the individual from enjoying the present or making clear decisions, resulting in procrastination and sleep deprivation. Their irritability strains relationships, and the physical symptoms of tension lead to chronic headaches and body aches, impacting their overall health and well-being.
Strategies to Try Before Seeking Treatment
Before anxiety or OCD symptoms become severely disruptive, there are practical strategies rooted in Cognitive Behavioral Therapy (CBT) principles that can help.
Strategies for Managing Anxiety (GAD)
- Schedule Worry Time: Instead of allowing worry to consume your entire day, designate a specific 15-minute period daily (e.g., 6:00 PM) for worry. When a worry arises outside this time, briefly jot it down and tell yourself, “I will worry about this later during my scheduled time.” This practice helps train your mind to contain the worry.
- Challenge Your Thoughts: When a “what if” thought appears, ask yourself:
- “Is this thought based on fact or feeling?”
- “What is the most realistic outcome, not the worst-case one?”
- “Is this worry helpful or productive right now?”
- Mindfulness and Body Scans: Practice taking a few minutes each day to focus entirely on your breath or to scan your body, noticing areas of tension without judgment. This grounds you in the present moment and helps distinguish between a stressful thought and physical reality.
Understanding Obsessive-Compulsive Disorder (OCD)
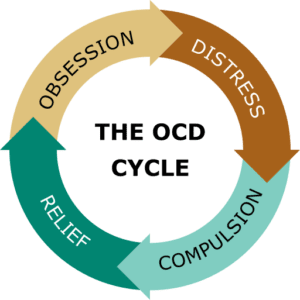
OCD is characterized by a two-part cycle:
- Obsessions: These are persistent, unwanted, and intrusive thoughts, images, or urges that cause intense distress, guilt, or disgust. They feel out of character and are not pleasurable.
- Compulsions: These are repetitive behaviors or mental rituals performed rigidly in response to an obsession, designed to reduce the resulting anxiety or to prevent a feared outcome.
The crucial difference is that the compulsion provides only temporary relief, which reinforces the cycle, teaching the brain that the ritual is necessary to keep the feared outcome at bay.
Real-World Examples of OCD Symptoms
OCD symptoms are not always obvious hand-washing or checking locks. They can manifest in subtle, yet debilitating ways.
Example 1: The Perfectionist Paralysis
A graduate student begins working on their thesis, a task that should take several weeks. An obsession surfaces: a feeling that their work must be “just right” or they will fail and be publicly humiliated. This translates into a compulsion to re-read every sentence, constantly editing for word choice, formatting, and minor logical inconsistencies, sometimes spending an entire day on a single paragraph. This behavior, known as “Symmetry” or “Just Right” OCD, is a form of checking compulsion.
- Problem Created: The individual’s perfectionism stalls their progress completely. The fear of being wrong is so overwhelming that the compulsion to repeatedly check and re-do the work leads to missed deadlines and academic paralysis.
Example 2: The Silent Mental Checker
A new parent develops an intrusive, horrific image of accidentally harming their child—a common theme in “Harm OCD”. They know they would never act on it, but the thought causes agonizing guilt and fear. The compulsion isn’t physical; it’s a covert mental ritual. They mentally review every interaction they’ve had with their child for the past hour, trying to confirm, “Did I do anything wrong? Am I a bad person?” They may also avoid being alone with their child to reduce the chance of acting out the fear.
- Problem Created: This internal checking and avoidance consumes their mental energy and joy. It creates a rift in the parental bond and causes severe emotional distress, leading to depression and extreme isolation from their primary support system.
Example 3: The Contamination Avoider
A young professional obsesses over an irrational fear of illness, specifically catching a rare and debilitating disease from public objects. The compulsion is to avoid specific “contaminated” items or places, like public transit or door handles in the office. They spend excessive time cleaning their workspace and may even use elaborate, ritualized actions to touch objects only with their elbow or sleeve.
- Problem Created: Their life shrinks dramatically. They can no longer take the subway, limiting job opportunities, and they struggle to eat out or visit friends. Their fear and resulting avoidance interfere with every facet of social and professional life, creating profound isolation and career stagnation.
Strategies for Managing OCD
- Identify the Cycle: Learn to recognize the exact sequence in the picture above: Obsession -> Anxiety -> Compulsion -> Obsession. Naming the components is the first step toward breaking the cycle.
- Delay the Compulsion (The “Time Out”): When an urge to perform a ritual strikes, try to delay it by a small, specific increment—even just one minute. Tell yourself, “I can do the ritual, but I will wait one minute.” Gradually increase the del
 ay. This creates a space between the urge and the action.
ay. This creates a space between the urge and the action. - “Unhelpful” Thoughts: When an intrusive thought (obsession) appears, mentally label it as an “OCD thought” rather than “my thought.” Acknowledge it—”That’s an OCD thought about germs”—and then refocus your attention on the present task. Do not engage with the thought or try to argue with it. This is a subtle form of Exposure and Response Prevention (ERP), the gold standard treatment for OCD.
Therapists for ocd near me
When It’s Time to Find a Therapist
While self-help strategies are valuable, there comes a point when professional intervention is necessary. It is time to seek professional help when:
- Impairment: Your symptoms significantly interfere with your ability to function in major life areas, such as work, school, relationships, or personal hygiene.
- Time: You spend more than one hour per day either worrying (GAD) or performing rituals (OCD).
- Distress: The emotional suffering, anxiety, or depressive feelings are intense and persistent, making daily life feel intolerable.
- Avoidance: You are actively avoiding people, places, or situations because of your fears, causing your life to feel constrained or “small.”
How to Find the Right Therapist
Finding a therapist who specializes in anxiety and OCD is crucial, as misdiagnosis or ineffective treatment can worsen symptoms. You can reach out to me, via the button below or via the contact form to set up a consultation. Alternatively, you can also follow these steps:
- Seek Specialization: Look for a therapist who explicitly lists Cognitive Behavioral Therapy (CBT), and specifically Exposure and Response Prevention (ERP) for OCD, in their credentials. ERP is non-negotiable for effective OCD treatment.
- Ask Targeted Questions: When you call for an initial consultation, ask: “What is your experience treating OCD/GAD?” and “Do you practice Exposure and Response Prevention (ERP) for OCD?”
- Use Directory Resources: Utilize professional directories like:
- The Anxiety and Depression Association of America (ADAA)
- The International OCD Foundation (IOCDF)
- Consult Your Primary Care Physician (PCP): Your PCP can often provide referrals to mental health professionals or prescribe initial medication to manage severe anxiety while you wait for a specialist appointment.
Accurate diagnosis is paramount. A skilled clinician will take the time to differentiate between the subtle ways anxiety and OCD manifest, ensuring you receive the specific, evidence-based treatment required for your condition. This journey begins with the courage to seek help and the resolve to reclaim your life from the cycle of worry and ritual.
Let’s Talk About What is Going On





